COVID-19 can’t stop recovery: Relationships between drug usage, COVID-19 isolation
When they enter the recovery scene, people are often told to buy a tuxedo because they’ll be burying their friends soon enough. While this sentiment is dark, it shines a light on an inconvenient truth about recovery: most people don’t recover from drug and alcohol substance abuse issues. According to an article about the discussion of substance and COVID-19 in the 2020 issue of Psychological Trauma, numbers have only gotten worse over the past year, as relapse rates and deaths have skyrocketed. I’ve personally seen several close friends either laid to rest or “gone out” in the past 12 months, and I attribute it mainly to the circumstances created by the pandemic. It is essential now more than ever to support those in recovery and encourage those struggling with substance abuse to seek help; be it via support groups or other treatment.
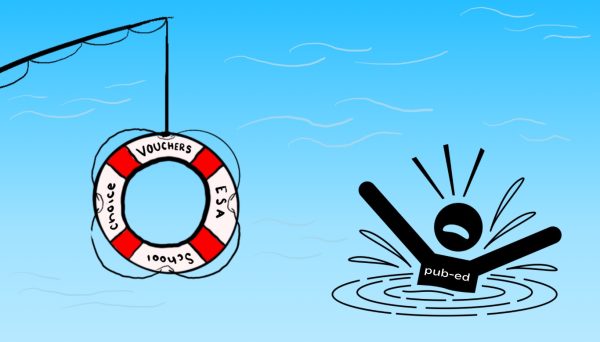
While this past year has been challenging for everyone, high-stress levels and disruption of “normal” life have been especially difficult for the addict population. According to the 2020 issue of Psychological Trauma, an article on COVID-19, opioid use and mental health says the difficulty is due to the compounding effect isolation has on an individual’s mental health. This population has been suffering in silence since it was deprived of the essential tools necessary to combat addiction. In many ways, COVID-19 was the perfect circumstance for addicts to exacerbate their use because the disease of addiction thrives in isolation. The pandemic provided substance abusers with low levels of accountability, restricted access to healthy coping skills and limited access to treatment options, it’s no wonder this population is struggling.
To make matters worse, people have been stuck inside, in many cases by themselves. It is not surprising that as a result of the pandemic, alcohol sales have doubled in the past year and opioid deaths have increased by 20,000 compared to the year prior (Psychological Trauma). Like many industries, the recovery community did attempt to adapt to the changing times by moving anonymous group meetings into the digital space; however, they proved to be less engaging. The consensus was that an essential human element was missing from this digital format.
Now I know what you’re thinking; these people who are relapsing are choosing to use again, but it is not that simple. Substance abuse, in general, can be a difficult concept to grasp if you’re not familiar with anyone battling addiction. Wouldn’t you offer a cancer patient your sympathy? So why don’t we do the same for substance abuse which is just as terminal? For addicts, it’s not a choice whether they use substances, especially if they don’t have the tools available to them to combat the insidious disease of addiction. Meetings, accountability, service work and fellowship with other addicts are the addict’s chemotherapy and it’s been taken away from them.
It is abundantly clear that in response to the pandemic, American society has normalized the importance of discussing mental health. This is a conversation that is far from over but has undoubtedly become more poignant during the pandemic. The pandemic has ironically allowed us the space to check in with one another in a much more meaningful way than before. We can now acknowledge the simple difficulty of being a human and the stress of life, and in doing so, help others find better paths before substance abuse becomes the path chosen.
I hope that the struggles of COVID-19 will not get overwritten as a fluke year, but that the normalization of mental health will be a seemingly small yet highly positive outcome of this hectic time in our generation’s growth. Hopefully, we can spend less time at funerals and more time supporting the populations of addicts because they have so much to offer this world.